Dr. Md. Rashidul Haque, MBBS, FCPS (Psychiatry)
Delirium is an acute, fluctuating, generalized cognitive impairment in which the patient has altered consciousness and disorientation.
We have to understand some basic terms to know about delirium and other cognitive disorders.
Organic: Psychiatric disorders which has a biological or chemical etiology are called organic (e.g., dementia, hepatic encephalopathy, uremic syndrome, etc.).
Functional: Those brain disorders with no generally accepted organic basis were called functional disorders (e.g., depression, schizophrenia, anxiety disorder, etc.).
Neuropsychiatry: It focuses on the psychiatric aspects of neurological disorders and the role of brain dysfunction in psychiatric disorders.
Neuropsychiatry is sometimes used interchangeably with Organic Psychiatry.
Organic Psychiatry: Neuropsychiatry + psychiatric disorders that arise from general medical conditions with their basis outside the brain (e.g. endocrine and metabolic disorders).
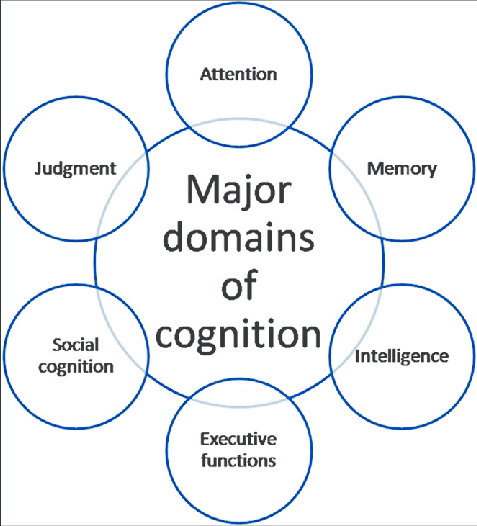
Cognition: Multiple domains of the brain include memory, language, orientation, judgment, conducting interpersonal relationships, performing actions (praxis), and problem-solving.
Cognitive disorders: Disruption in one or more of the above domains, and are also frequently complicated by behavioral symptoms.
Synonymous of Delirium:
Intensive care unit psychosis/Acute confusional state/Acute brain failure/Encephalopathy/Toxic metabolic state/Central nervous system toxicity/Paraneoplastic limbic encephalitis/Sundowning syndrome, Cerebral insufficiency/Organic brain syndrome.
Epidemiology:
The prevalence of delirium in the elderly is 1-2% in community samples. It is much more common elderly than for younger people. In the community studies, age 55 years or elder 1% & age 85 years and older 13% develop delirium.
Prevalence in General Medical setting – 10-30%, Emergency department – 7-10%, Orthopedic surgery patients – 33%, Open heart surgery patient – 30%, Post operative patients – 15-53%, ICU units – 70-87%, End of life care – 83%, Severe burns -21%, AIDS patients – 40%, Terminally ill patients – 80%.
Clinical features:
Altered consciousness & disorientation in time and place. (Hallmark of delirium)
Impaired attention.
Often psychomotor hyperactivity and hypoactivity.
Emotional disturbances, Anxiety, irritability, depression, and emotional lability.
Thought –Disorganization of thought processes (ranging from mild tangentiality to frank incoherence). Muddled thinking.
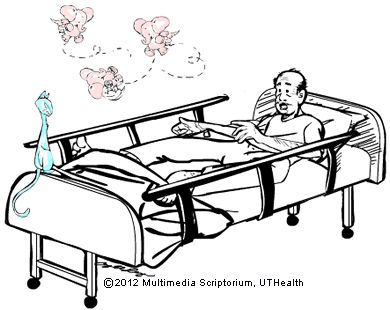
Perceptual disturbances –Illusions & hallucination (visual and auditory hallucinations).
Neurological symptoms –Autonomic hyperactivity or instability, myoclonic jerking, dysarthria, tremor, asterixis, nystagmus, incoordination, and urinary incontinence are common.
Sleep disturbances –Disruption of the sleep-wake cycle (often manifested as fragmented sleep at night, with or without daytime drowsiness).
• Risk of delirium
Predisposing factors:
Age 65 years and older
Male sex
Cognitive impairment
or Dementia. Sensory impairment
Dehydration
Severe medical illness
Neurological diseases
Treatment with drugs with anticholinergic properties.
Alcohol abuse
Chronic renal & hepatic disease
Metabolic derangement
Terminal illness
•Precipitating factors:
Drugs – ü Sedatives-hypnotics ü Anticholinergics ü Narcotics ü Polypharmacy ü Alcohol or drug withdrawal
Inter-current infection – üInfections (e.g. UTI, RTI) üSepticaemia üHypoxia üShock üSevere acute illness üAnaemia üFever or hypothermia üDehydration üPoor nutritional status üLow serum albumin
Primary neurological diseases- • Stroke • Meningitis • Encephalitis
Surgery –
Environment- • Admission to ICU • Use of physical retrains • Use of bladder catheter • Pain • Emotional stress • Prolong sleep deprivation
Etiology: